The COVID-19 pandemic has altered the normal operation of European hospitals since March 2020, and stroke care has not been an exception. Patients, professionals as well as hospital care routines have all suffered the consequences.
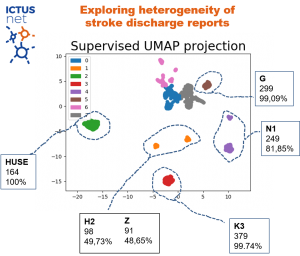
Health authorities, public health professionals, doctors, nurses and other health professionals suddenly changed the way they were used to work and focused all their efforts on fighting the pandemic. The ICTUSnet project was no exception, and the work of the beneficiaries was focused on real-time data analysis, evidence assessment and, finally, safe care of COVID-19 and non-COVID-19 patients according to the resources available at any time. Multiple ICTUSnet project activities were postponed until the epidemiological situation allowed them to continue.
The stroke care chain has been altered for several reasons, firstly, at the prehospital level, due to:
- saturation in emergency services,
- delays in seeking medical care at the onset of symptoms because of late identification of the disease as a consequence of social distance
- delays in calling emergency systems for fear of being infected by SARS-CoV2
- showing stroke symptoms together with respiratory symptoms of Covid19
Secondly, at the hospital level, due to:
- the overload of the emergency department
- the need to adapt the action protocols
- the need to establish a protected stroke code and to know the infectious status of the patient to place him in a safe space.
Initially, professionals did not have all the necessary protection measures. Some of them became infected, some for long periods of time. They have also suffered stress and, in addition, the care overload has prevented attention to other non-care tasks.
On the other hand, although the main symptoms of coronavirus infection are respiratory, it has been detected that cerebrovascular disease can be a clinical manifestation of COVID because the increased risk of vascular events in these patients. and stroke COVID related could be more severe with poor outcomes.
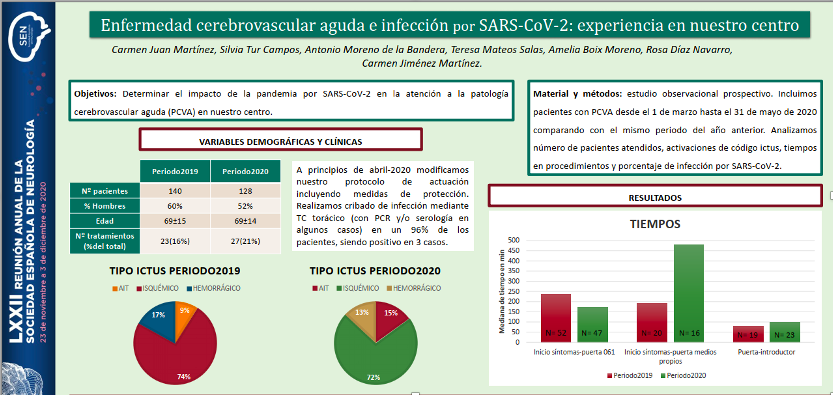
At the Universitary Hospital Son Espases (IdISBa partner), we have compared stroke care from March 1 to May 31, 2020 to the same period of time from previous year founding no differences in the number of patients seen nor in the number of cerebral reperfusion treatments performed in the ischemic stroke; we did detect an increase symptoms onset time upon arrival at the hospital in those patients who came to the hospital on their own, and also in the time from arrival at the hospital to the start of mechanical thrombectomy (door-introducer), attributed to the established safety protocol.
Today our work has been adapted to guarantee excellent care for patients affected by cerebrovascular disease, whether or not they are infected with SARS-CoV2, and to provide the maximum safety measures for healthcare professionals and patients.
The impact of the pandemic on the care of each region has been different depending on: COVID-19 incidence, stroke incidence, and health resources adaptation dedicated to this pathology (e.g. critical beds have been able to include stroke unit beds).
For all above mentioned, it is likely that Covid 19 has affected the ICTUSnet project not only in its execution, with the deadlines extension , but also in its result (e.g. WP1 takes into account the action times).